|
<< Click to Display Table of Contents >> Understanding the Billing Workflow |
  
|
|
<< Click to Display Table of Contents >> Understanding the Billing Workflow |
  
|
| A. | Insurance Charge Workflow |
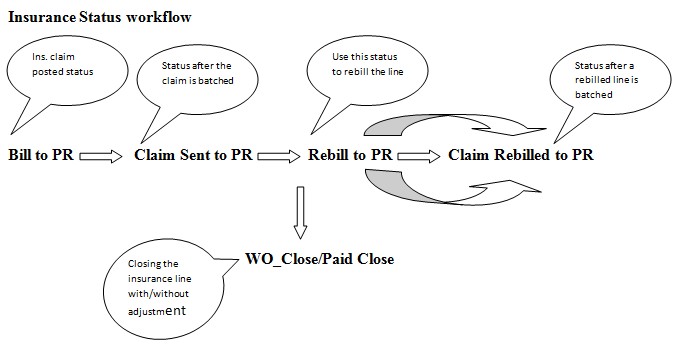
Any new insurance charge is always posted with the status – “Bill to PR” (abbrev. for Bill to Primary Insurance). Bill to PR status would indicate to the user that the claim was posted, but hasn’t yet been submitted. Additionally, any charge crossed over from EHR to the billing would appear in a “NEW” status on the Enter Charges screen. Save the charge with status Bill to PR to post the charge.
After the first batch & submission of the claim, the line status is changed by the system to “Claim Sent to PR”. This indicates the claims was batched and submitted once.
Use the “Rebill to PR” line status to refile a claim. The line status would be changed to “Claim Rebilled to PR” on the next batch or subsequent refiling and batching of the claim. A charge if in “Rebill to PR” indicates that the claim/line hasn’t yet been batched after it was put to the rebill status.
The same workflow would apply to Secondary or Tertiary claims. The status for the secondary claims would begin with “Bill to SE” and for tertiary – “Bill to TR”.
When a batching is done, all the claims sitting in Bill to PR(/SE/TR) & Rebill to PR (/SE/TR) are pulled up by the system for batching to electronic batch/paper depending on their method of submission.
An open line can be closed with/without an adjustment. If there is no adjustment, the line status is closed with a “Paid Close” status. If there’s an adjustment on the line, the line can be closed with a “WO Close” status.
If there is a balance on an insurance charge, the line status can be moved to a Bill to PT or Bill to GR status while applying the payment or from the Edit Charges screen.
| B. | Patient/Guarantor Charge Workflow |
Any patient bill can be posted with a “Bill to PT” (abbrev. for Bill to Patient) or “Bill to GR” (abbrev. for Bill to Guarantor) status. The former status is used when the patient is the responsible party and statement needs to go out to the patient. If the responsible party is the Guarantor, use the Bill to GR status.As in the case of an insurance line posting, the Bill to PT lines can be closed with a “Paid Close” or “WO Close”.