|
<< Click to Display Table of Contents >> Print Claims |
  
|
|
<< Click to Display Table of Contents >> Print Claims |
  
|
1) Click on the Billing module and Choose the Claims Work Bench menu to open Claims work bench.
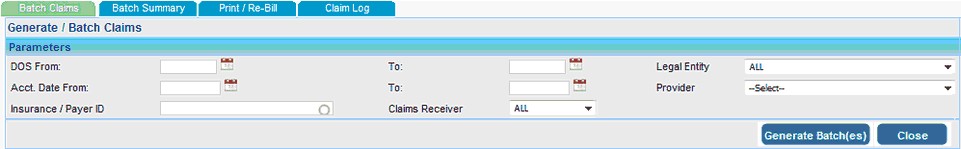
2) Click the ![]() button with out selecting any parameters to generate all claims in our system. Use the parameter like DOS From - To, Acct. Date From - To, Legal Entity, Provider, Insurance and Claims Receiver to filter the claims which is to be generated.
button with out selecting any parameters to generate all claims in our system. Use the parameter like DOS From - To, Acct. Date From - To, Legal Entity, Provider, Insurance and Claims Receiver to filter the claims which is to be generated.
3) Click the ![]() button to submit the claims, which will take to Batch Summary tab.
button to submit the claims, which will take to Batch Summary tab.
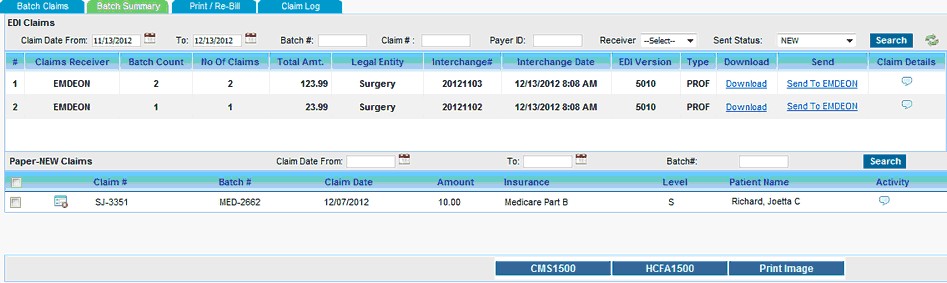
4) The Batch Summary tab lists the EDI Batch Interchange and Paper New Claims.
a) EDI Batches can be downloaded by clicking on the Download link or can send to the clearing house by clicking on the Send To link.
b) Paper New claims can be printed in 3 formats
| • | CMS 1500 |
| • | HCFA 1500 |
| • | Print Image CMS 1500 |
5) Click on the Print/Re-Bill tab in order to Print/Reprint/Re-bill selected claims.
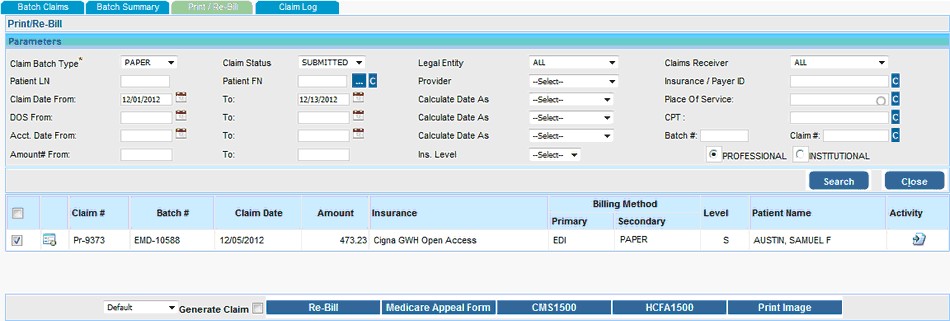
Use the Parameters like Claim Batch Type, Claim Status, Legal Entity, Claim Receiver, Patient Name, Provider, Insurance, Claim Date From-TO, DOS From-To, Acct. Date From-To, Amount From-To, Place Of Service, CPT, Batch#, Claim#, Claim Type, Insurance Level etc to search the claims.
Claims will be listed below on clicking Search button according to the given parameters.
Encounter Line details of the claim can be viewed by clicking on the ![]() icon near to Claim#. Claim Activity can be viewed by clicking on the
icon near to Claim#. Claim Activity can be viewed by clicking on the ![]() icon under the Activity column.
icon under the Activity column.
6) Select the claim(s) from the list.
a) The selected claims can be be printed in 3 formats by clicking on respective buttons listed below.
| ➢ | CMS 1500 |
| ➢ | HCFA 1500 |
| ➢ | Print Image CMS 1500 |
b) You can also generate a Request for Redetermination of Medicare Claim by clicking the Medicare Appeal Form button.
c) The selected claims can be re-billed by clicking the ![]() button. To generate the re-billed claims from this screen itself select the Generate Claim check box before clicking on the
button. To generate the re-billed claims from this screen itself select the Generate Claim check box before clicking on the ![]() button.
button.
7) Select the Claim Log tab to view the Claim Detail Report which provides the claims details.
8) Upload the ANSI Claim Response file under Claim Response tab under Claim Log to view the claim response is an readable format.